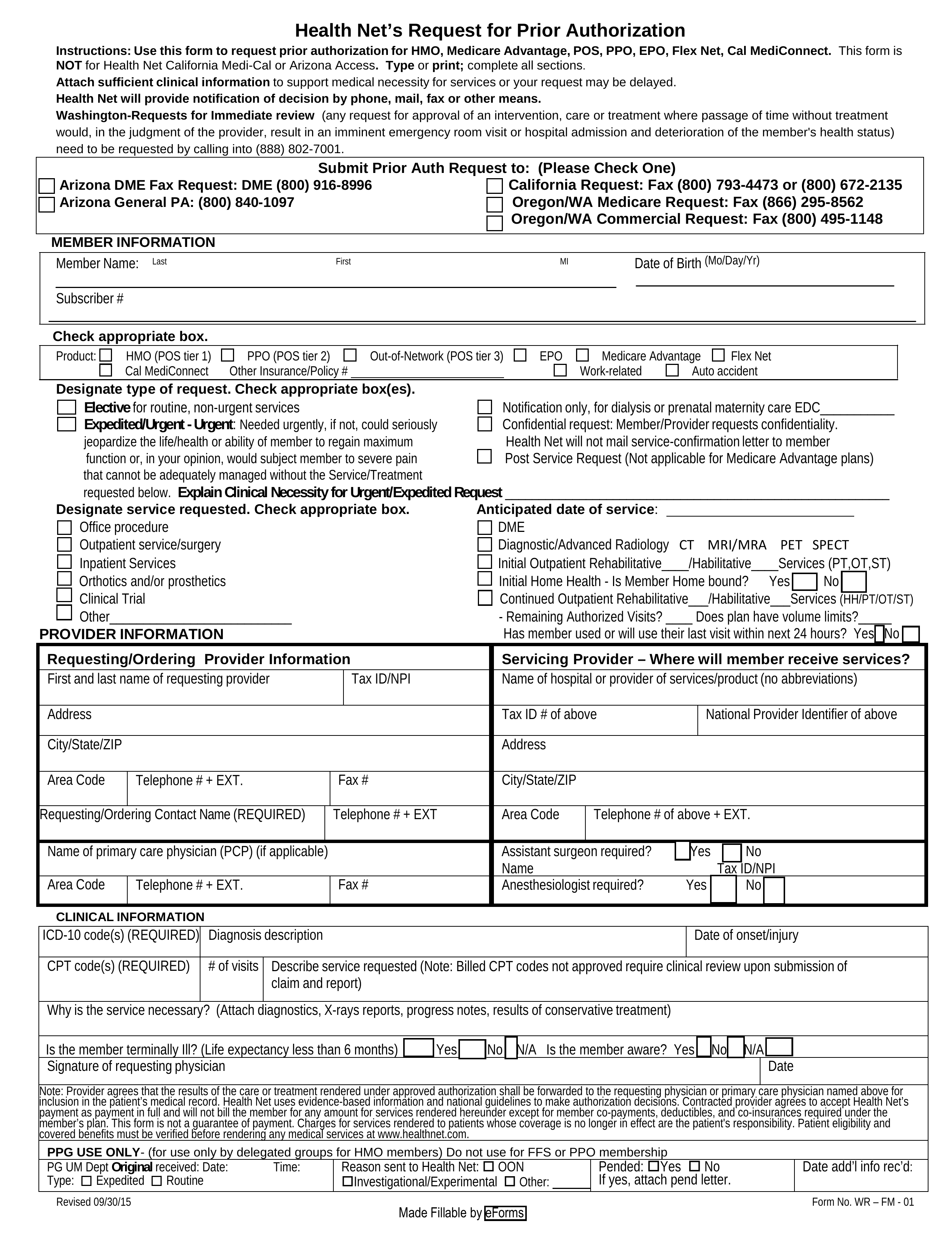
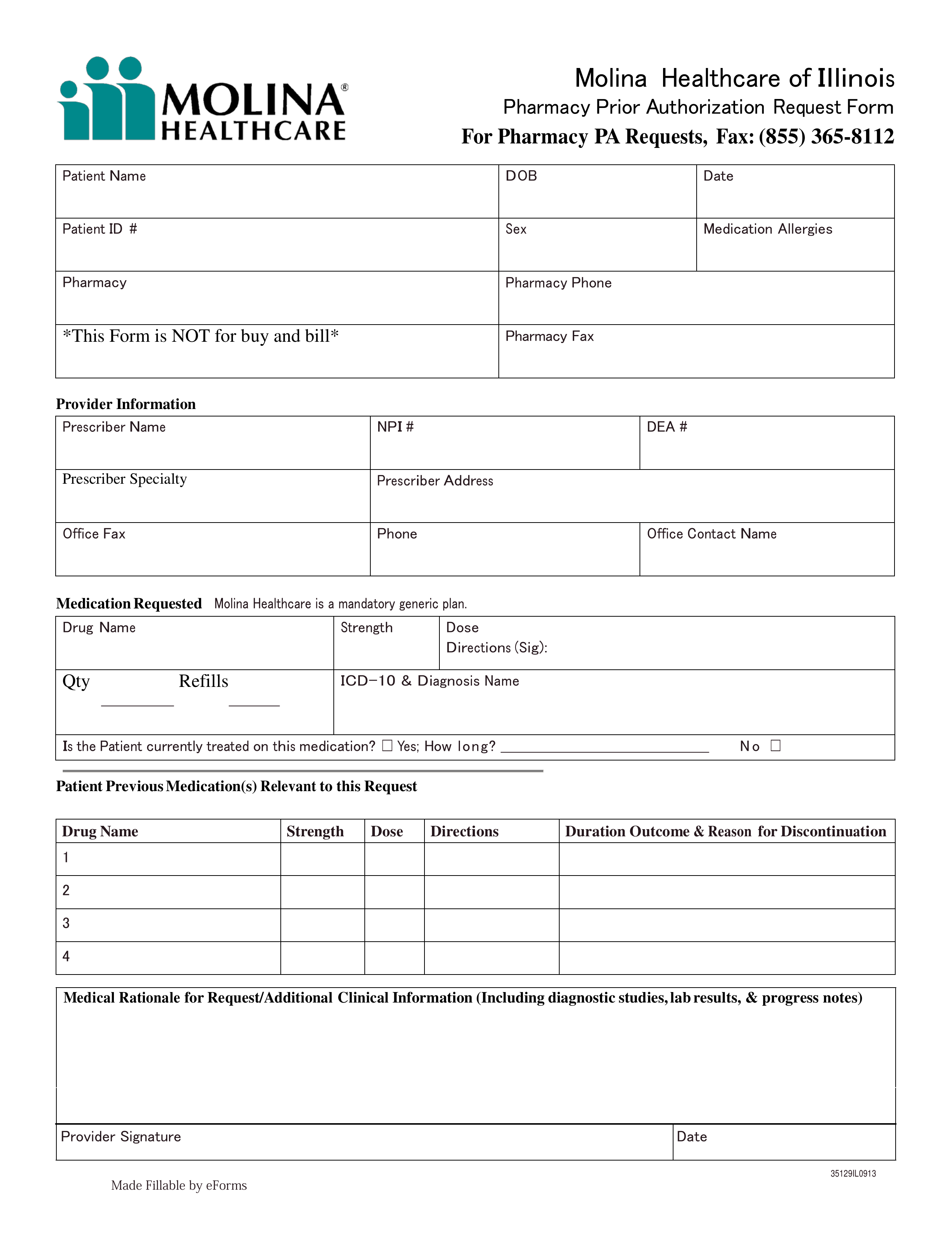
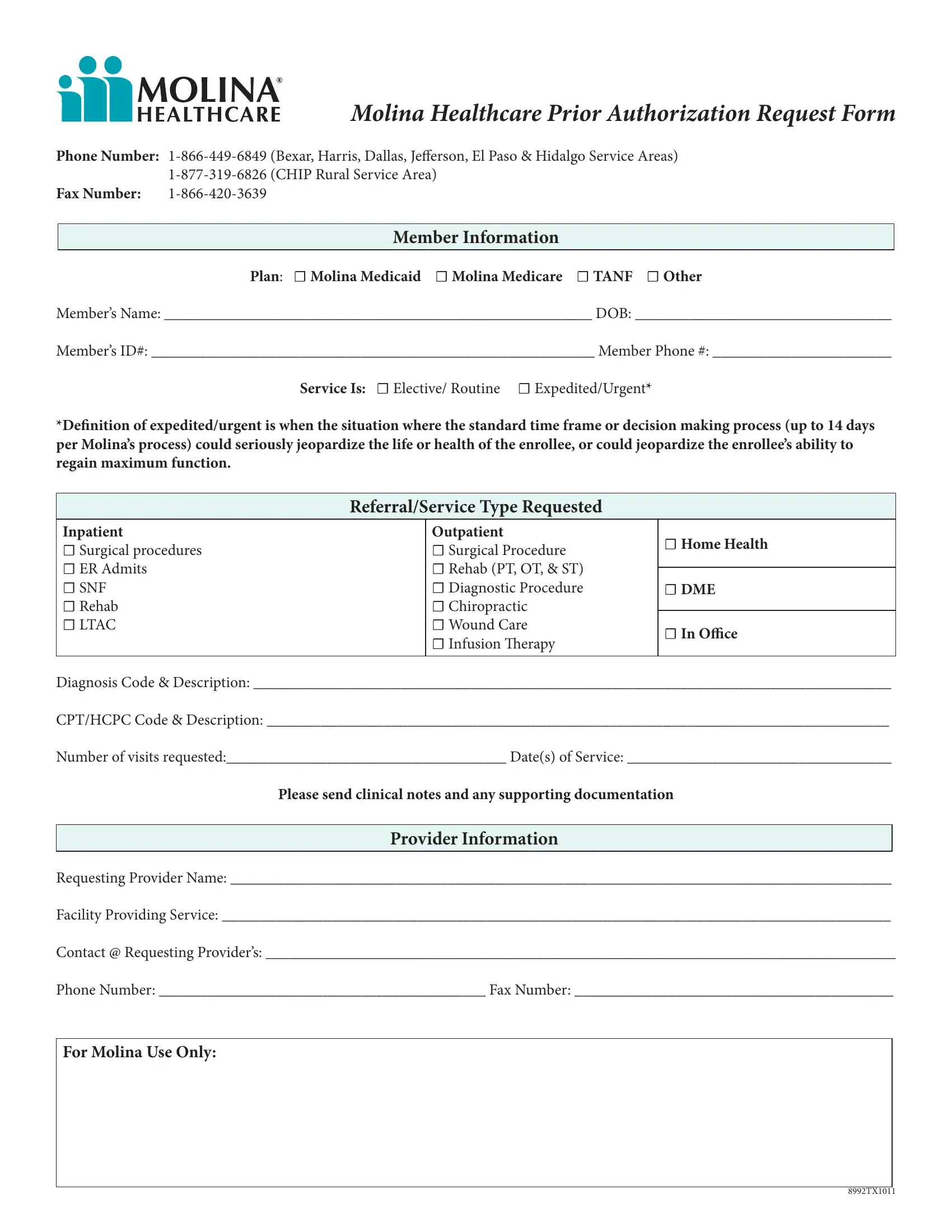
Webprior authorization is when your provider gets approval from molina healthcare to provide you a service. It is needed before you can get certain services or drugs. Providers may utilize molina’s provider portal: Claims submission and status. Webshould an unlisted or miscellaneous code be requested, medical necessity documentation and rationale must be submitted with the prior authorization request. For mmp medicaid, please refer to the. Refer to molina’s provider website/prior authorization. For dual members with medicaid, please. Refer to molina’s provider website or prior. Providers may utilize molina’s provider portal: Claims submission and status.
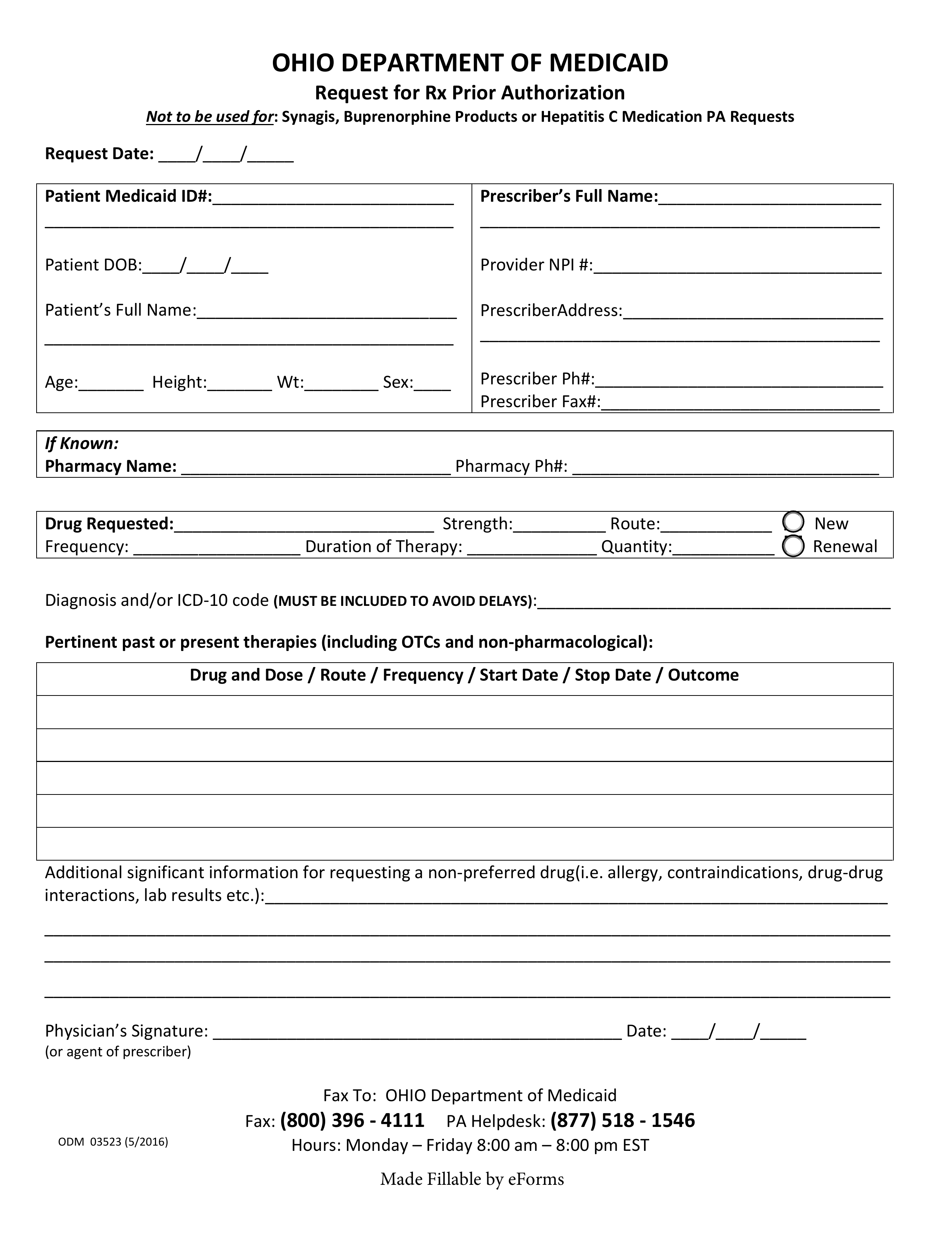
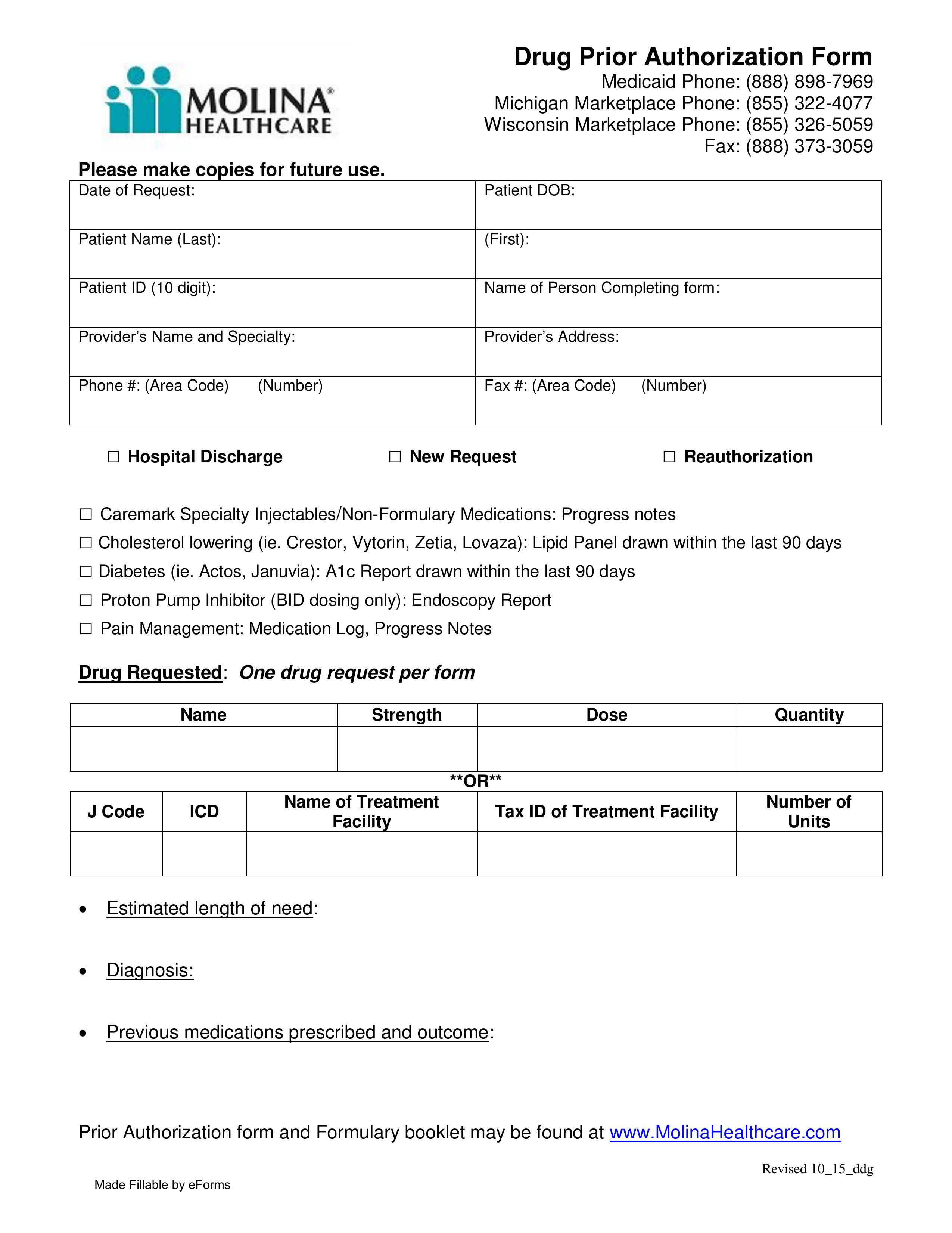
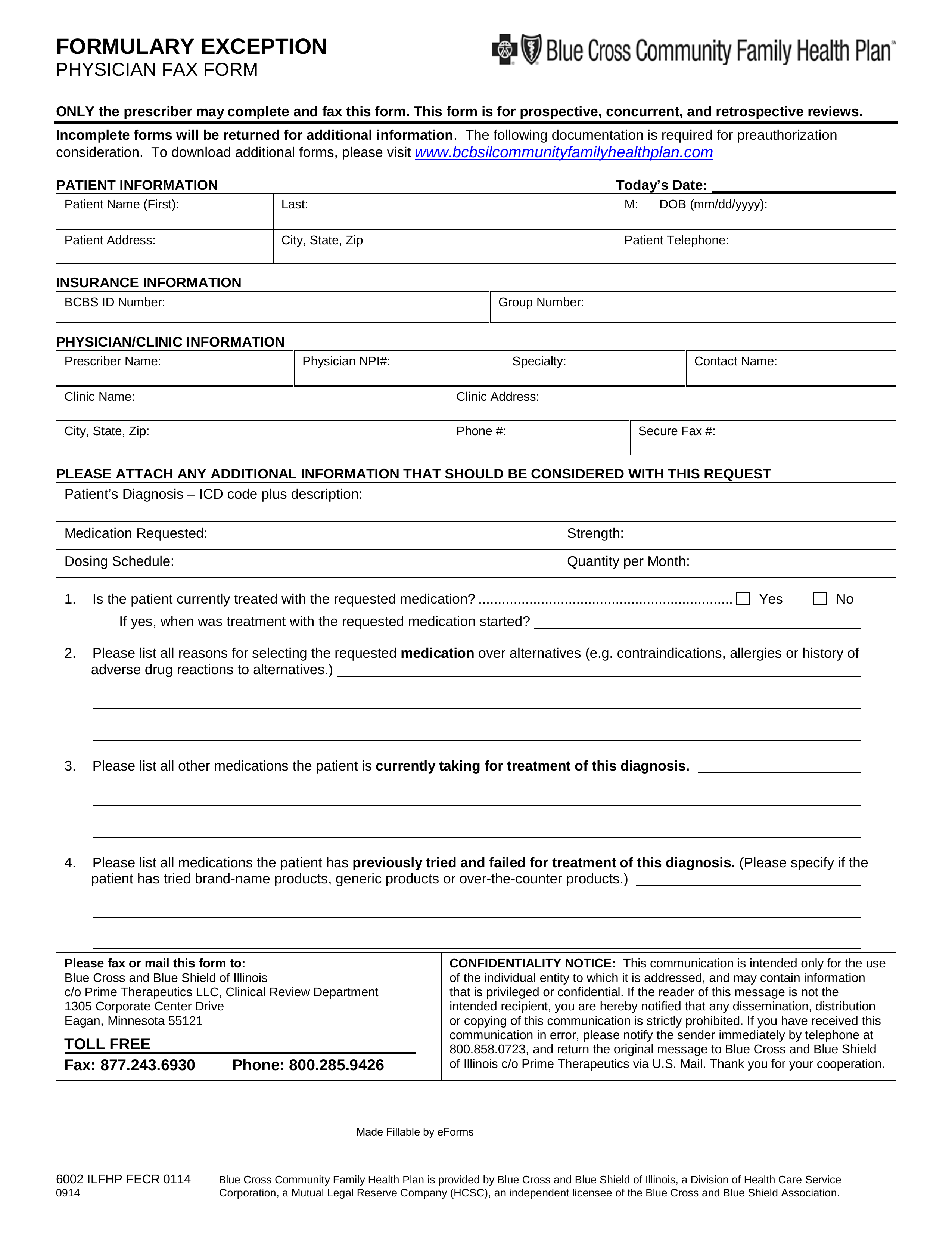
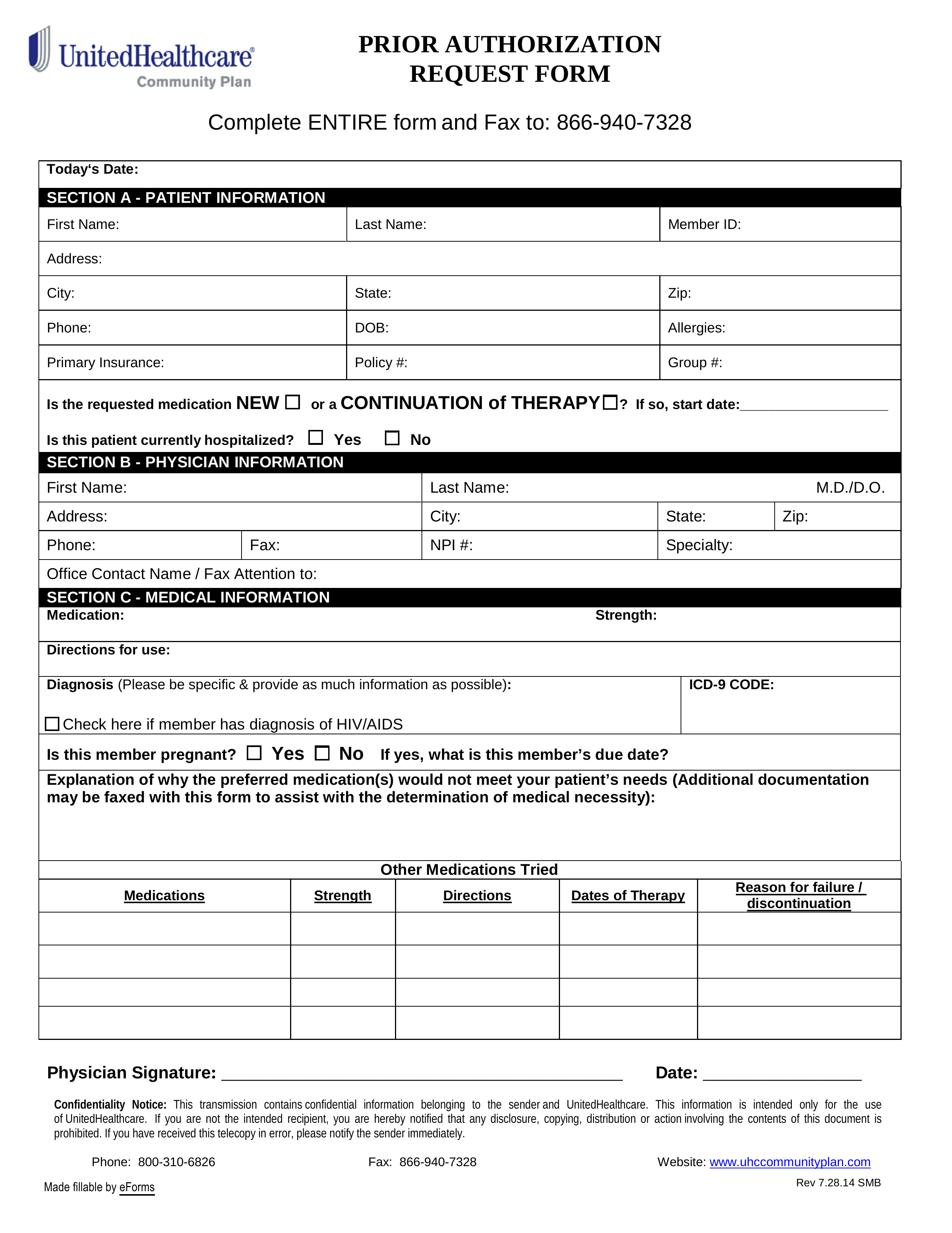
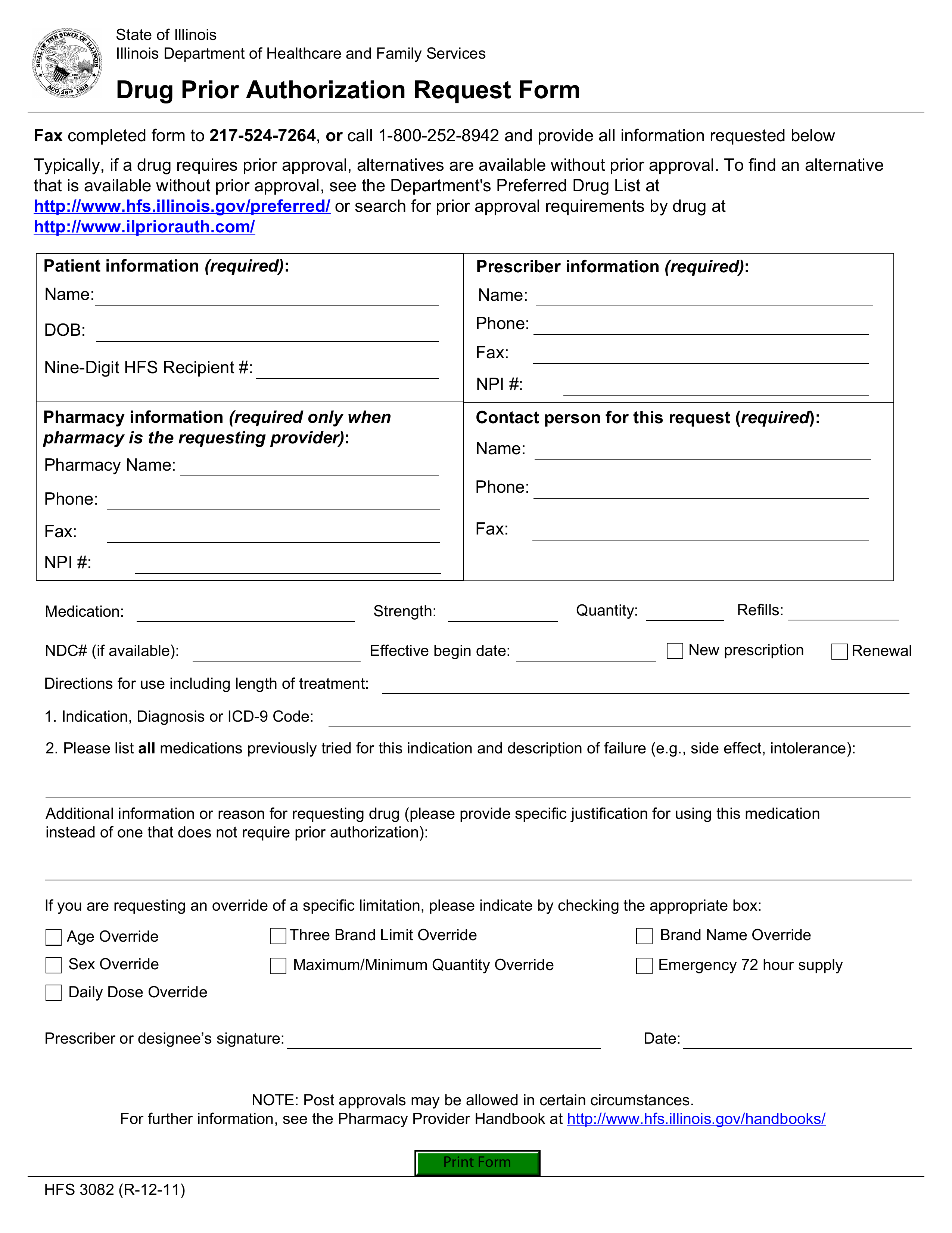
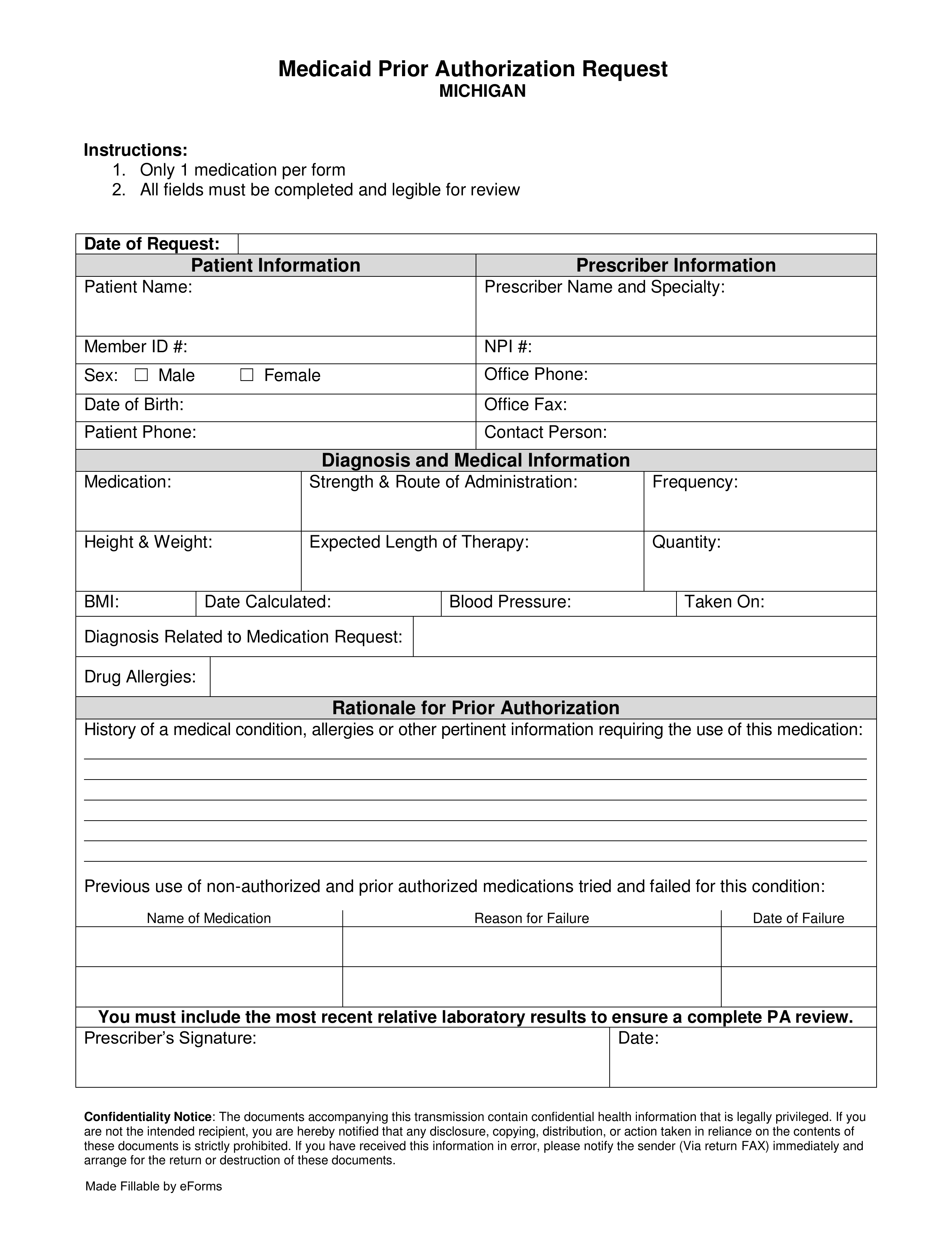
MedicaidPrior Auth Form
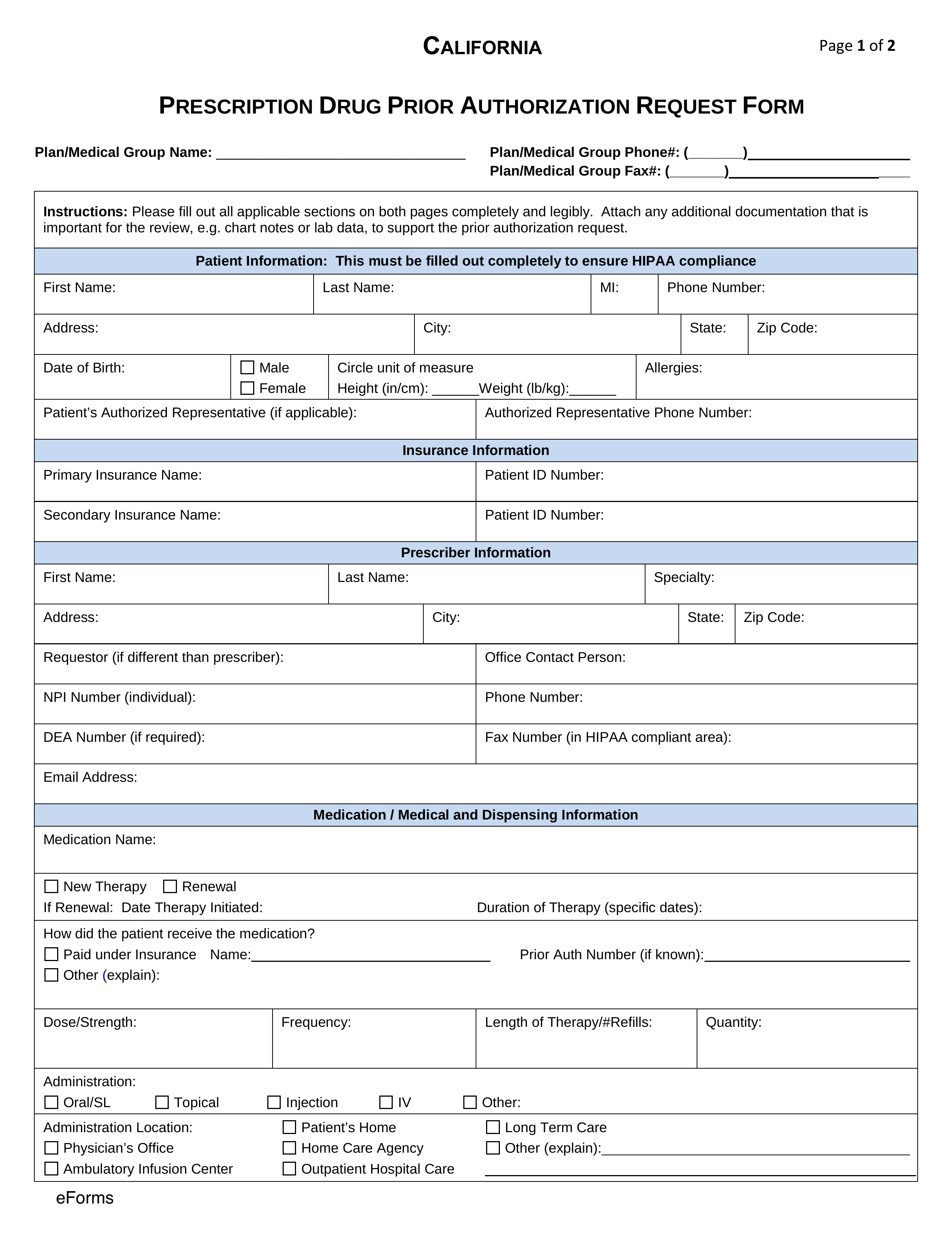
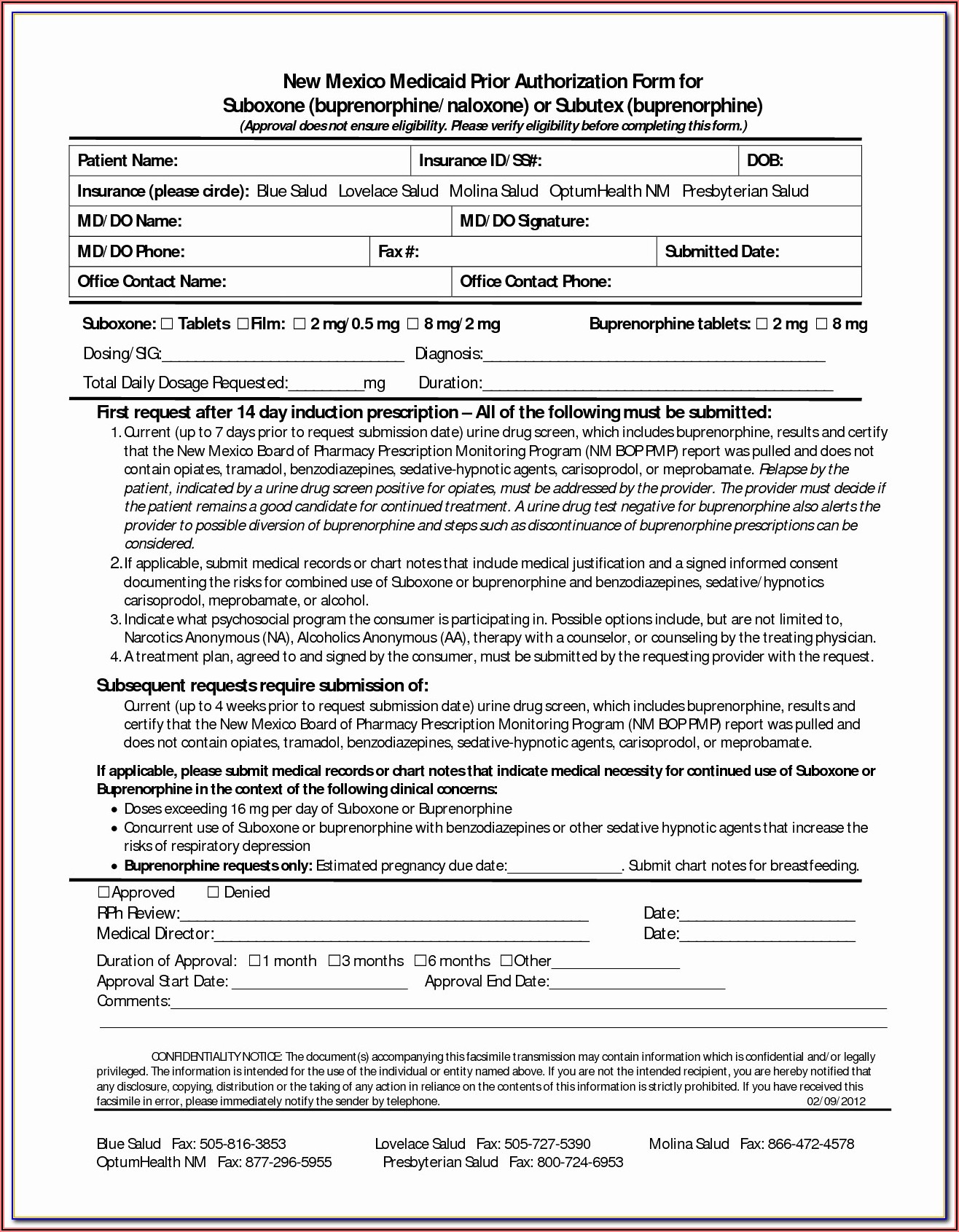
Molina Medication PriorAuthorization Form
Prior Authorization Formsfor Molina
Molina HealthCare PriorAuthorization Form
Molina Insurance PriorAuthorization Form
Molina PriorAuthorization Form California
Molina Pharmacy PriorAuthorization Form
Molina Prior AuthForms30156tx0213
Molina Prior AuthSheets
Molina PriorAuthorization Form PDF
Molina PriorAuthorization Request Form
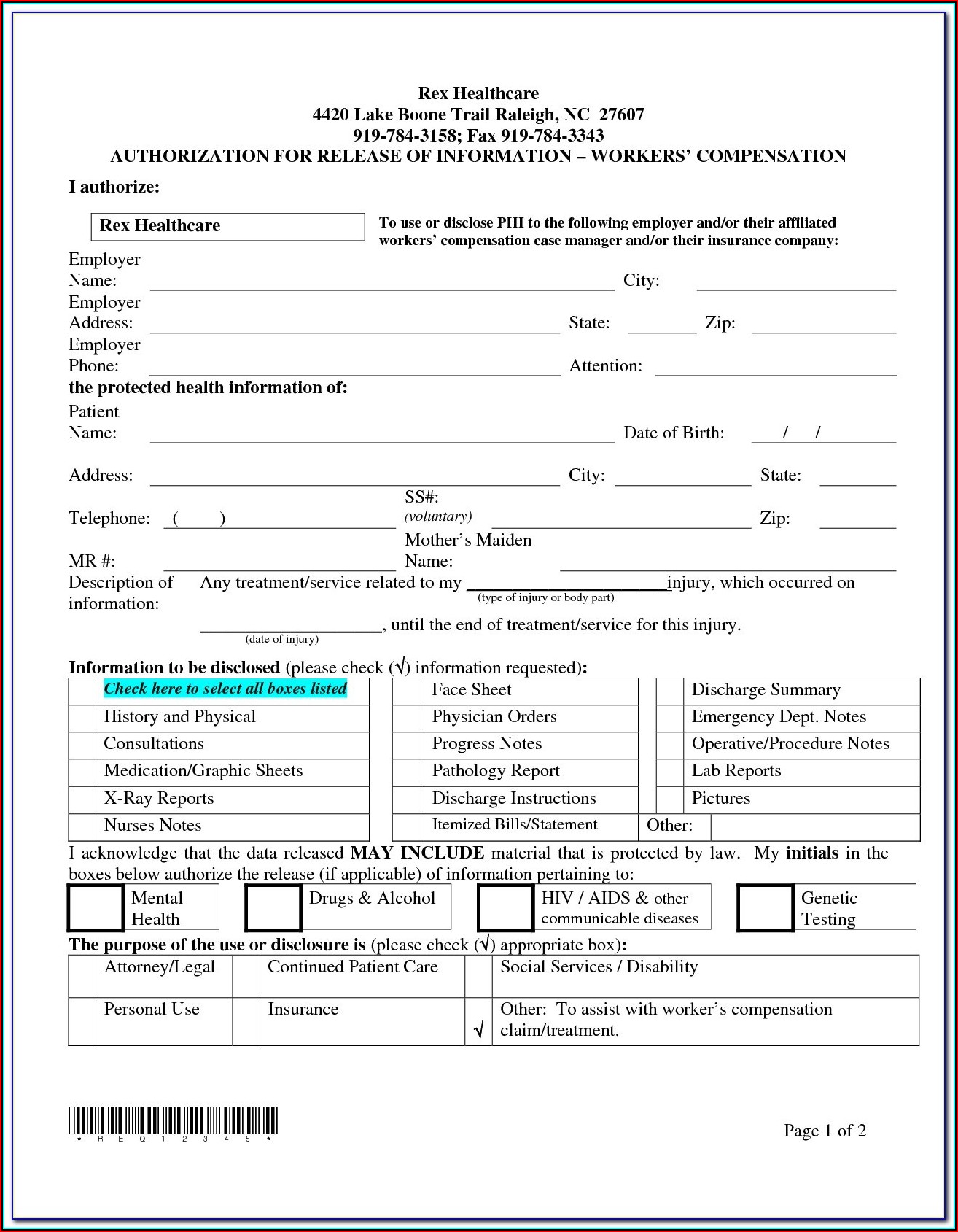
Surescripts Prior Auth FormPrintable
Molina Prior Auth Formfor Iowa